
A large study examined the association between implementation of state-mandated sepsis protocols, compliance, and mortality. Sepsis standard operating procedures, initially specified as Early Goal Directed Therapy have evolved to “usual care” which includes a standard approach with components of the sepsis bundle, early identification, lactate, cultures, antibiotics, and fluids. Standard operating procedures are a set of practices that specify a preferred response to specific clinical circumstances.

However, while there is wide variation in sensitivity and specificity of sepsis screening tools, they are an important component of identifying sepsis early for timely intervention. A pooled analysis of three RCTs did not demonstrate a mortality benefit of active screening (RR 0.90 95% CI 0.51–1.58). Screening tools may target patients in various locations, such as in-patient wards, emergency departments, or intensive care units (ICU). Machine learning may improve performance of screening tools, and in a meta-analysis of 42,623 patients from seven studies for predicting hospital-acquired sepsis the pooled area under the receiving-operating curve (SAUROC) (0.89 95% CI 0.86–0.92) sensitivity (81% 95% CI 80–81), and specificity (72% 95% CI 72–72) was higher for machine learning than the SAUROC for traditional screening tools such as SIRS (0.70), MEWS (0.50), and SOFA (0.78). A variety of clinical variables and tools are used for sepsis screening, such as systemic inflammatory response syndrome (SIRS) criteria, vital signs, signs of infection, quick Sequential Organ Failure Score (qSOFA) or Sequential Organ Failure Assessment (SOFA) criteria, National Early Warning Score (NEWS), or Modified Early Warning Score (MEWS). There is wide variation in diagnostic accuracy of these tools with most having poor predictive values, although the use of some was associated with improvements in care processes.
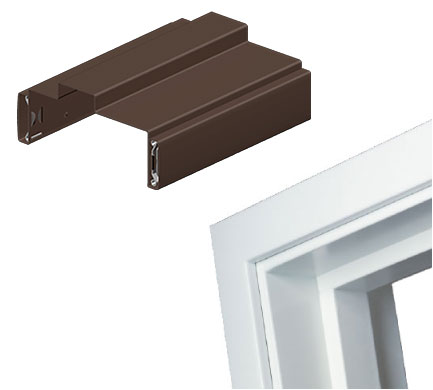
AMS TIMELY DOOR FRAMES MANUAL
Sepsis screening tools are designed to promote early identification of sepsis and consist of manual methods or automated use of the electronic health record (EHR). The specific components of performance improvement did not appear to be as important as the presence of a programme that included sepsis screening and metrics. Despite some inconsistency, a meta-analysis of 50 observational studies on the effect of performance improvement programmes showed that these programmes were associated with better adherence to sepsis bundles along with a reduction in mortality (OR 0.66 95% CI 0.61–0.72) in patients with sepsis and septic shock. Sepsis performance improvement programmes generally consist of sepsis screening, education, measurement of sepsis bundle performance, patient outcomes, and actions for identified opportunities. Strong recommendation, very low-quality evidence for standard operating procedures

Strong recommendation, moderate quality of evidence for screening For hospitals and health systems, we recommend using a performance improvement programme for sepsis, including sepsis screening for acutely ill, high-risk patients and standard operating procedures for treatment

Intensive Care Medicine volume 47, pages 1181–1247 ( 2021) Cite this articleġ. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021


 0 kommentar(er)
0 kommentar(er)
